The anterior cruciate ligament (ACL) connects the thigh and shin bones and is critical in providing stability to the knee joint. The ACL is most commonly injured during sporting activities leading to anterior and rotatory instability of the knee. The primary function of the ACL is to prevent the tibia (shin bone) from sliding out in front of the femur (thigh bone) and provides rotational stability to the knee. ACL tears are most often managed by reconstruction. That is, the torn tissue is removed with a shaver and a new ACL (autograft or allograft) is inserted into the knee. However, recently there has been a resurgence of interest in primary repair of the ACL in select patients.
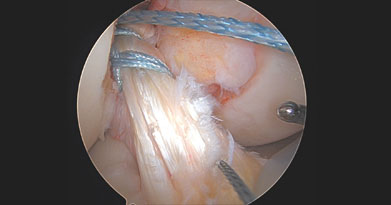
In select patients, one may elect to proceed with a primary repair of the torn ACL with a minimally invasive arthroscopic procedure to repair the ligament. When an ACL is repaired, the surgeon places sutures in the remaining ACL stump and fixates this suture back towards the bone from which the ACL should attach to. Typically, this procedure is considered for patients with a more proximal (femoral or “thigh” bone) avulsion tear (the ligament is pulled away from the bone) with a good quality ligament stump still attached to the tibia. Figure 1 demonstrates placement of sutures in an ACL that was found to be approximately 80% intact with the proximal 20% wall attachment compromised. This tear was repaired and tensioned with sutures as shown in Figure 2. A biologic that can help the ACL heal includes bovine collagen via the BEAR procedure (Bridge Enhanced ACL Repair). A blood clot is inserted surrounding the ACL to facilitate its healing. Benefits of ACL repair include smaller incisions, avoidance of donor site morbidity and thus preserved strength, maintained proprioception or balance fibers in the ACL, and less arthritis. Dr. Momaya was the first orthopedic surgeon in the state of Alabama to repair a torn ACL repair with the novel BEAR procedure. However, ACL repair failure rates do remain unsatisfactory in those who are higher demand athletes and younger aged patients when compared to ACL reconstruction (Cruz, 2023).
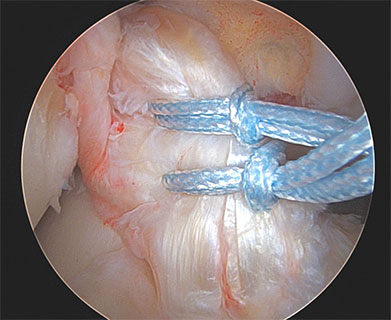
Figure 1
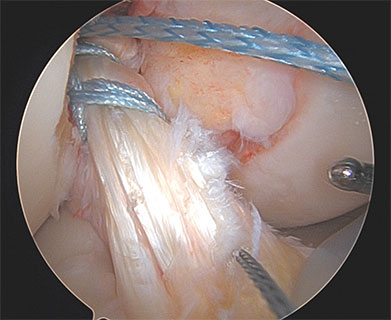
Figure 2
Notably, the quality of the ACL remnant is often influenced by the chronicity of the ACL tear. Most ACL repairs should generally be performed within several weeks after the initial injury. This timeline increases the likelihood the ACL remnant can be properly reattached to its anatomic origin. If an ACL injury is amenable to repair, your surgeon may also discuss a non-biological augmentation to the repair. This is typically completed in the form of a high strength suture which reinforces the repair and is often referred to as an “internal brace.”
Compared to ACL repair, ACL reconstruction refers to the torn ligament being completely substituted with either autograft (tissue from your own body) or allograft (donor tissue). Historically, ACL reconstructions have been shown to result in superior functional outcomes and survivorship in comparison to ACL repairs (Benedict, 2019). In general, ACL reconstruction is indicated in active individuals in which the ACL is not amenable to repair (Evans, 2023). Figure 3 shows a complete mid-substance ACL rupture that was reconstructed with a quadriceps tendon autograft (Figure 4).
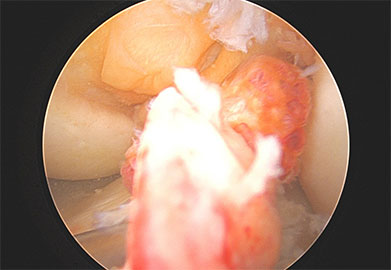
Figure 3
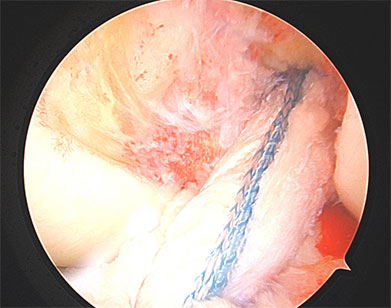
Figure 4
In summary, ACL reconstruction refers to removing the torn ACL and using a new graft for the ACL. In contrast, ACL repair refers to preservation of your torn ACL and repairing it with suture. ACL repairs are generally reserved for acute injuries involving the proximal portion of the ligament making patient selection a critical factor in managing these injuries. Both options should be discussed with patients seeking surgical management for an ACL tear. Please call and schedule an appointment with a board-certified orthopaedic surgeon who specializes in sports medicine when deciding which treatment is best for you.